Literature versus clinical practice: rehabilitation intervention after subacromial decompression and rotator cuff repair
Posted on 1st October 2019 by Nicolò Garzetti
Introduction
The aim of this blog is to compare the exercises performed during daily clinical practice against what the literature suggests for rehabilitation interventions after subacromial decompression and rotator cuff repair.
Clinical case report
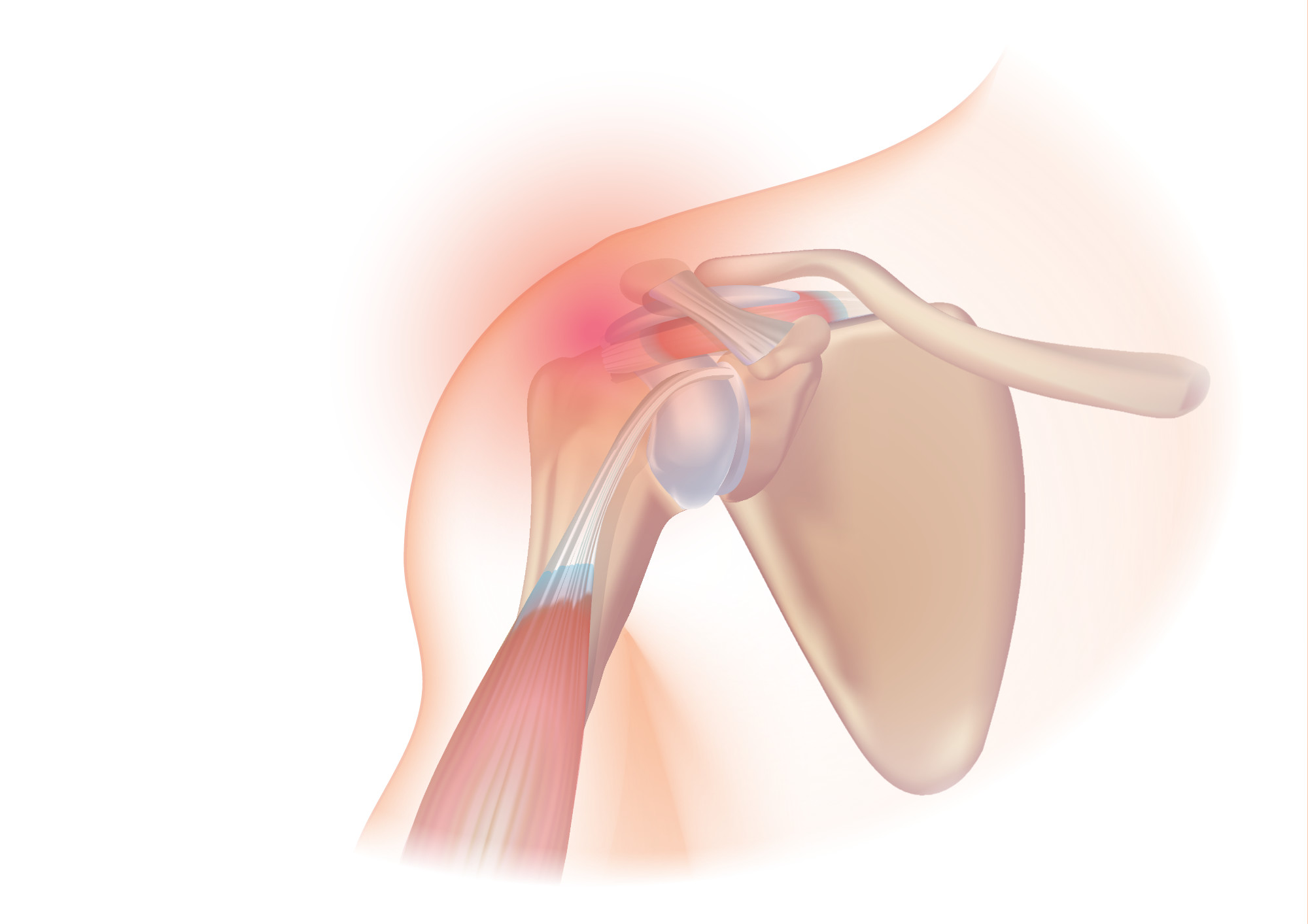
The patient was a 60-year-old woman who experienced pain in her left shoulder while lifting a weight during her job in August 2018. She reported persistent pain in her left shoulder since then. Her doctor referred her for a Magnetic Resonance Imaging (MRI) which showed deposits in the joint fluid, clavicular and acromion arthrosis, supraspinatus tendon degeneration and swelling to the biceps longhead tendon. An ecographic analysis confirmed supraspinatus tendon degeneration and highlighted limitations in the sub-acromial joint.
The patient underwent surgery of an arthroscopic subacromial decompression and rotator cuff repair in November 2018. In the months before surgery, she did not perform any conservative treatment.
6 weeks after surgery, the patient presented with active range of motion (ROM) to 100° with compensatory movement, and passive ROM of 120°. Active and passive abduction ROM was 90°, and internal and external rotation ROM was 30°. Pain had decreased (Numeric Rating Scale (NRS) = 4/10) compared to the period before surgery (NRS= 8/10), but still persisted.
The focus of treatment at this point was the recovery of active and passive ROM of the shoulder in all movements and pain control.
What does the literature suggest?
In the literature, there are different surgical and non-surgical methods cited for the treatment of rotator cuff tears. Generally, in clinical practice, if the pain does not go away by itself or with various treatments like steroid injections, physiotherapy, or both, surgery becomes the most suitable choice. However, the literature is conflicting in its conclusions. Karjalainen et al [1] investigated the effectiveness and safety of surgery in the treatment of rotator cuff disease of the shoulder, concluding that:
the data does not support the use of subacromial decompression in the treatment of rotator cuff disease manifest as painful shoulder impingement. High‐certainty evidence shows that subacromial decompression does not provide clinically important benefits over placebo in pain, function or health‐related quality of life.
Beard et al [2] confirm these findings, stating that the clinical evidence in favour of this type of shoulder surgery is still scarce. Considering the questionable value of this surgery type, this should be communicated to patients during the shared treatment decision-making process. Therefore, the physical therapy could be considered as first line of treatment. When arthroscopic cuff repair is used, early passive mobilisation aimed at decreasing postoperative stiffness and improve functionality is suggested, making sure not to compromise repair integrity [3].
Passive mobilization and physical therapy
Rehabilitative treatment after rotator cuff repair (immediately after surgery until 4-6 weeks post-op) is based on patient education, shoulder immobilisation with an abduction pillow for 4-6 weeks unless specifically directed to do otherwise by the surgeon, and active and passive motion of the elbow, wrist, hand and cervical spine in order to avoid any possible immobilisation syndrome.
Grubhofer et al [4] showed how to monitor objectively the compliance rate of wearing the shoulder brace with temperature-sensitive sensors. Passive ROM exercises should be performed with gentle pendulum oscillations. There are many forbidden movements in this phase, such as: lifting heavy objects, pushing and pulling, excessive shoulder extension and rotation movements, stretching or sudden movements, and supporting the body weight with elbow or hand during transfers. During this period, cryotherapy at home is suggested and, if possible, aquatic rehabilitation in order to maximize the range of motion in a safe environment [5] .
During the first rehabilitation phase, different electrotherapy methods, like interferential currents, TENS and ultrasound, can be used to reduce pain. There are similar improvements between these different techniques in terms of pain relief, function and quality of life four weeks after the treatment and at three months post-op. However, interferential current treatment provided significantly better outcomes in the mental component of quality of life [6].
Pain free passive and active-assisted mobilization and isometric exercises
Between 4-8 weeks after surgery, if painless passive motion, passive forward flexion to at least 110° – 125°, passive external and internal rotation in arm immobilizer to at least 25°-45° and passive glenohumeral abduction in arm immobilizer to at least 90° are achieved, it is possible to introduce, alongside passive mobilisation, active-assisted mobilisation exercises to improve neuromuscular control and strength, while at the same time minimizing pain and inflammation symptoms. Moreover, in this time, sub-maximal isometric exercises for external and internal rotation can be initiated; these exercises are performed holding the arm below shoulder height, elbow flexed to approximately 90°, and held in a neutral rotation position.
Stretching exercises and elastic resistance activities
From 10-12 to 16-18 weeks post-op, with full active ROM and no signs of scapular-thoracic dyskinesia, the strengthening phase can start with stretching and strengthening exercises in order to improve muscle power and endurance. These exercises are external rotation, internal rotation, forward flexion and rowing motion. Free exercises can be used to strengthen the biceps and triceps muscles.
Advanced strengthening
In the period between 16-26 weeks after surgery advanced, strengthening should take place.
It is important to choose specific exercises that target the scapular stabilizing muscles. To ensure high levels of infraspinatus and teres minor strength, external rotation of the shoulder at 45° of abduction utilizing elastic bands can be performed, moving to external rotation exercises at 90° of abduction in order to activate supraspinatus muscle and, finally, upper limb plyometric exercises, which for example include a patient throwing and catching a weighted ball against a wall, starting at shoulder height and progressing gradually to the overhead position. These exercises are meant to improve neuromuscular control and strength.
Conclusion
The literature highlights that subacromial decompression does not provide clinically important benefits over placebo in terms of pain, function or health‐related quality of life. This suggests that the reason guiding surgeons over the decades should be revisited, and the differences between surgical vs conservative treatment could be the result of the placebo effect, postoperative physiotherapy with associated rest or other effects. In conclusion, physiotherapy should be the first choice of treatment, associated or not with the surgery, for pain relief and the improvement of function, ROM, strength and quality of life.
References (pdf)
Image credit: ‘Rotator cuff syndrome’ by Injurymap is licensed under CC BY 4.0