Economic analysis part 1: an introduction to the topic
Posted on 1st October 2021 by Ana María Rojas Gómez

This is the first of a three-part blog which will provide an introduction to economic analysis (part 1), an explanation and examples of the different types of economic evaluation (part 2), and a more detailed look at a few aspects of the topic (part 3).
What is economic analysis?
Public health authorities and clinicians increasingly use methods that allow appropriate resource allocation and maximum benefit for the patient. In other words, effective and efficient use of resources. Therefore, they have to conduct a comparative analysis of competing alternatives. This must include identifying, measuring, and valuing the consequences and costs of the interventions being considered (1) (figure 1). Economic analysis in health is also known as the economic evaluation of health care.
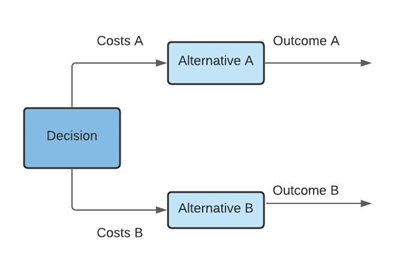
Figure 1. Decision analysis in health economic evaluation
Opportunity cost
Economic evaluation is not about money but is the value of what you lose when choosing between two or more options (opportunity cost) (figure 2). For example, a new alternative might reduce the time a health provider must spend on a particular activity or disease. This can release a scarce resource but doesn’t release health provider time. In fact, there may well be no money savings because health providers reallocate that time to other health-improving alternatives. The health provider can now achieve more with their ‘released time’ for the benefit of society, but there are no financial savings.
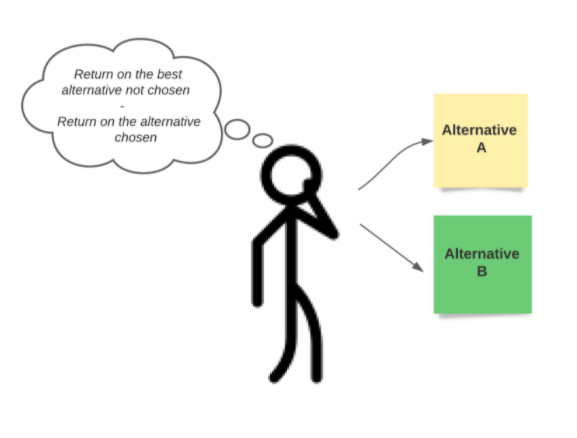
Figure 2. Opportunity cost
Perspective
Considering that an economic evaluation is conducted mainly to report results at national levels according to the country or location, we should also take into account the ‘perspective’. In this context, perspective is the viewpoint assumed for the analysis of costs and outcomes. It may come from one, or a group of patients, a health institution, society, or a third-party payer, for example (figure 3).
Perspective allows us to determine the costs and benefits of each of the alternatives. When we are interested in the costs of providing health care services, such as the cost of medications or costs of inpatient treatment, we may be considering a third-party payer or health institution perspective. If our interests include out-of-pocket costs, that is, expenses for health care that aren’t reimbursed by insurance, we may be considering a patient perspective. Lastly, if we include all expenditures generated by the intervention and we take into account providers and potential beneficiaries at the same time – to measure fully the wider benefits to society – we are considering a social perspective.
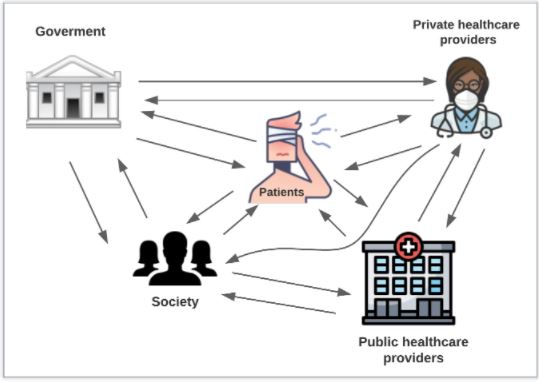
Figure 3. Health actors to consider in the perspective
Timeframe
An economic evaluation of health must also consider the timeframe of analysis – time of use of the new intervention, and the time for which costs and benefits will continue to generate value, such as survival gains. The time horizon depends on the nature of the disease and intervention. For example, a life-time horizon will be preferred to obtain short- and long-term effects on health and costs, including potential long-term side-effects or benefits in a chronic condition, like diabetes. A shorter time horizon may be preferred for some acute conditions, such as acute respiratory infections.
Level of evidence
In addition, the level of evidence needs to be borne in mind as this clearly has an important influence on the results. The clinical question should ideally be answered by high-quality evidence (figure 4). Guidelines recommend using systematic reviews of randomized controlled trials, one or more RCTs, or a non-randomized controlled study whenever possible, although sometimes RCTs can differ from real-world clinical data. So, consideration should be given to appropriate clinical data to answer the clinical questions (figure 4).
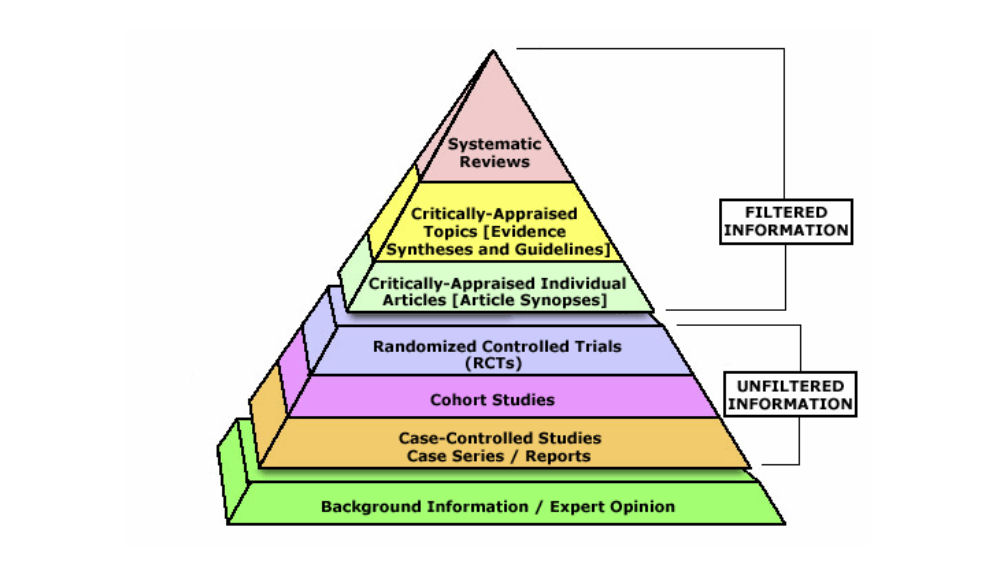
Figure 4. Evidence-Based Medicine Pyramid.
EBM Pyramid and EBM Page Generator, copyright 2006 Trustees of Dartmouth College and Yale University
In summary
The reality is, we do not have an endless pot of money to spend on health care. Our aim is to provide the maximum benefit to patients, and to do that with efficiency and effectiveness. That’s where health economic analysis comes in.
Against a background of increasing demands on limited resources, health economics is exerting an influence on decision making at all levels of health care. Health economics seeks to facilitate decision making by offering an explicit decision making framework based on the principle of efficiency (6).
In the following blogs…
… we will discuss the different types of economic evaluation and look deeper into key aspects of these analyses. Every evaluation differs, mainly in how we view outcomes:
- Cost-effectiveness analysis – when we consider a clinical effect of interest observed by a health professional, common to both interventions but obtained to different degrees, for example, reduction in blood pressure or strokes averted;
- Cost-minimization analysis – when interventions are identical in the effect of health outcomes;
- Cost-utility analysis – whether perceived health benefit using the alternatives is included;
- Cost-benefit analysis – the costs and benefits of interventions quantified in common monetary units.

