Poor health literacy and its implications among the general population
Posted on 9th January 2023 by Ifedolapo Adejumo

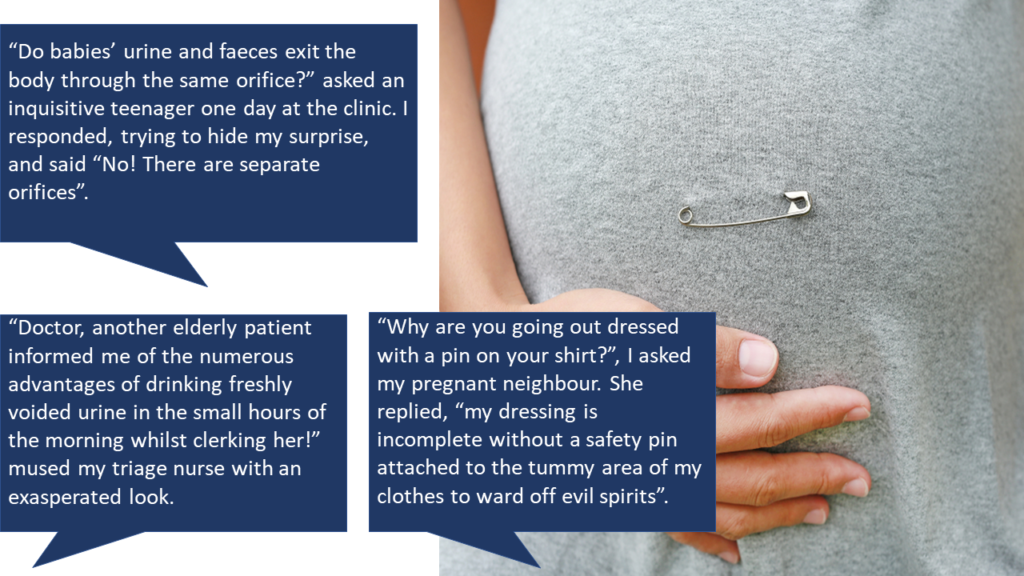
To begin, let me mention a few stories that I have heard in my over a decade-long clinical practice in the developing world…
An introduction to health literacy
Health literacy is, in a nutshell, the extent to which individuals can obtain, process, and understand basic health information and services needed to make an informed health decision [1].
It can be a proxy for health statistics in determining impactful health interventions by representing numerical statistical variables as an assessment criterion when making health decisions. However, it is noteworthy that health literacy is multidimensional in its various components such as cultural and conceptual knowledge, listening, speaking, arithmetical, writing, and reading skills [2].
According to a study by McClintock et al, peculiarities among countries with the accompanying cultural diversity and population indices must be taken into consideration when evaluating health literacy, keeping in mind the many variables that impact different individual experiences [3]. Hence, evaluation of health literacy cannot be divorced from inter-country variabilities, particularly culture and population indices.
There is evidence to support the factors influencing health literacy which include culture and belief system, poor and ineffective communication (language barrier), socio-demographic variables (age, sex, gender, ethnicity, religious affiliation, level of income, education, marital status, employment), socio-political, psychosocial, physical health status, and low socioeconomic status [4,5].
As an example, it was reported in Tai’s paper that “traditionally Asians, such as Chinese or Hindu individuals, believe that people are sick because their inner and outer forces are out of balance. According to the Chinese approach, the purpose of medicine is to restore the balance of Yin and Yang within a body”. [6]
To what extent does low health literacy impact health outcomes?
Health research as shown by Atulomah et al [7] demonstrated that low health literacy in some communities in the South West region of Nigeria could limit health utilization and therefore impede optimal health service delivery.
Low health literacy is characterized by the parameters which determine the understanding, acceptance, application, and utilization of health information, in the maintenance of health and prevention of diseases. Studies have shown a correlation between poor health literacy and poorer medical adherence, low life expectancy, poorer health status and disease outcomes, frequent hospital admission and readmission, and high morbidity and mortality, amongst others [8].
Most health-related obstacles faced by resource-poor countries with high health illiteracy are due to rapid population growth [9]. A good knowledge of contraceptive use, for example, may help by preventing unwanted pregnancies and reducing maternal mortality [10].
Myths, misunderstandings, and misconceptions under the umbrella of health illiteracy were confirmed in a face-to-face review by Osungbade et al on “Epilepsy in a rural community in West Africa”, where over 80% of the study population attributed epilepsy to witchcraft, and 80% preferred treatment using a traditional approach which included herbal preparations (without scientific evidence of safety and efficacy), spiritual exorcisms, charms, and sacrificial offerings [11].
The health implication of this is that poor health literacy throws up additional complications arising from wrong and harmful practices and remedies, delay in seeking effective remedies, and worsening severity of illnesses, in addition to the primary disease.
Furthermore, it was identified in a country-specific assessment conducted in Zambia that young, married women on average had lower rates of health literacy (24.5% of the sample) compared to men (46.5%) [12]. Suffice to say, in the developing parts of the world, gender inequalities disallow female education and, by extension, access to health information and the empowerment required to put the acquired health information to use. This was the inference revealing a replica of the happenings in that specific area.
This was similar to a cross-sectional survey in developing countries like Isfahan where it was revealed that approximately 79.6% of adults had inadequate health literacy and the factors responsible for the majority of the population were low educational and socioeconomic status, as well as being female [13].
In addition, studies from Sao Paulo, Brazil concluded that 31.7% of people were found to have limited functional health literacy [14]. This was in tandem with a comparative analysis of literature where it was suggested that health literacy in developed countries like Japan is lower than that of Europe, and 75 million adults in the US are estimated to possess basic and less than basic health literacy [15,16].
A study conducted in Europe reported that at least 1 in 10 Europeans have an inadequate health literacy level [17]. In addition, approximately 90 million adults in the US (reported by the Institute of Medicine) stumble into a quagmire while assessing and understanding health information leading to unnecessary healthcare cost for the economy [18].
One cannot help but refer to one of the defining eras of the world in the COVID pandemic where accurate dissemination of information to the grassroots in rural Africa was of great importance as it affected disease outcomes. The dire consequences of a breach in information dissemination affected the rate of virus spread, awareness to comply with preventive precautionary measures (hygiene and facemask), presentation to health facilities in severe cases, quarantine, and self-medication with all sorts of self-acclaimed remedies of the disease.
The lack of access to the current trend of the disease progression on the media channels (print, social media, or web) had a great influence on the adoption of standard practices by the rural community as advocated by health practitioners. This closed the gap between “health messages” and the high patronage of unverified information from “health messengers” who do not have the disadvantage of a language barrier.
A US study concluded that people with inadequate health literacy have higher hospitalization rates and most of them fall in the age range of 70 to 79 years. The same study also reported an association of low health literacy with poor health maintenance, poor health care seeking, and higher rates of complications [19]. However, a literature review suggests that health literacy is still better in developed countries than in developing countries where limited studies on health literacy data are a challenge.
There are tools available for assessing functional health literacy including REALM, TOFHLA, NAAL and Adult literacy and Life tool (ALL), and the most modern adaptable tool for health care settings called Newest vital signs (NVS) which assesses reading ability and numeracy skills [20]. The European Health Literacy Survey Questionnaire (HLS-EU-Q) is another tool aimed at measuring and comparing health literacy in some selected European countries [21].
So, what can be done to help improve health literacy in the general population?
To improve the health implications of illiteracy, an effective patient-physician relationship will have to be built starting with the training and awareness of the issue with medical students. Health information in resource-poor countries (especially in the rural areas) may want to explore communication channels to disseminate messages such as radio, television, audiotapes, and videotapes expressed in the language they understand rather than written format. This may help users to comprehend medical information irrespective of their literacy status. Emphasis should be on ensuring the knowledge translates to a positive attitude and practice.
In developed countries, individuals should be encouraged to make use of online resources such as electronic health records, patient portals, and telemedicine options to elicit information that they can apply to their own informed health decisions.
Healthcare providers have a responsibility for using formats that can reduce misunderstanding of information by removing language barriers and other complexities. This may ease comprehension of medical instructions, prescriptions, and health services.
In conclusion, effective response to the issue of poor health literacy by easily accessing, discerning, evaluating and implementing information in tasks regarding health decisions, disease prevention, and health promotion could achieve better health behaviour.
References (pdf)
Further resources
You may also be interested in this blog on Evidently Cochrane which is aimed at anyone making health decisions. Sarah Chapman looks at some key things that can help you make a choice that feels right for you – Making health decisions: things that can help
There is also this course on ‘Lifeology’ which will help guide you in putting health literacy into action – How to Create Actionable and Engaging Patient Education. Lifeology have many beautifully illustrated, science-backed, bite-sized “flashcard” courses so do go and check these out.
An Informed Health Choices project have devised a list of ‘Key Concepts’ to help people think critically about whether to believe a treatment claim and what to do. Based on a previous version of this list, Students 4 Best Evidence bloggers have written a series of blogs which explain and expand on these concepts: Key concepts for addressing treatment claims.



No Comments on Poor health literacy and its implications among the general population
Thank you Dolapo for this well written piece. Let me add to the important point on patient-physician relationship: this alone, traditionally can help to overcome 80% of the problems association with poor health literacy. However, the current strictly business styled healthcare practice models is making it increasingly difficult for a long lasting doctor-patient relationship to be established.
Frequent migration of physicians, from one hospital to another, from one State to another and in recent times, from one country to another has real been the bane of effective patient-physician relationship.
Time, which is money, has been the fulcrum on which the balance tips. Many specialist Physicians and Surgeons would like to have a business-like dealing with the patients. They can only afford the time needed to educate patient on the particular ailment on the table, and see no reason to dwell on others health issues that are not immediately related to the diagnosis of discussion.
This approach helps in freeing enough time for them to attend to many other patients waiting in line to have access to them.
One would hope, that the leadership in the developing Nations like Nigeria and other African countries will pay attention to the training of more Family Physicians, who by their nature of training have the capacity and capability to stay rooted in a particular community where they can provide continuous, vertical and longitudinal care for as many people in the community from cradle to grave.
The patients are open to listening to, and adopting information given to them by a physician they share a long relationship with.
In addition, the provisions for the undergraduate training in Family Medicine is very sparse in Nigeria. The Universities need to do more. Medical students should have the opportunity of being exposed to the tenets of Family Medicine practice right from their early clinical years.
15th January 2023 at 8:49 amMuito Bom, muito bom e encorajador …
14th January 2023 at 1:58 pmThank you for this piece, Dr Adejumo. Interestingly you mentioned ‘communication channels’ to aid dissemination of health information. I have always found it interesting that In a place like Nigeria where poverty plays a huge factor towards affordability of healthcare. Yet many have mobile phones, social media and access to the internet. Health information and access to electronic medical records is a largely untapped resource in Nigeria. The importance of grassroots advocacy in improving health literacy cannot be overemphasized also.
9th January 2023 at 7:46 pmEnlightening piece, Thank you.
9th January 2023 at 6:54 pmA interesting and engaging read.
9th January 2023 at 6:45 pmVery educating. I learnt a few things here. Very done.
9th January 2023 at 12:36 pmVery insightful.
9th January 2023 at 11:47 am